

Increasing the adoption of new and proven healthcare treatments by overcoming the emotional barriers of fear and disgust.
Fear is a natural human biological response. It acts sort-of as an alarm clock that warns us to tread with caution and leads us away from risk, such as walking alone on a dark alley after midnight. We think twice about these kinds of things.
Yet it is often in the defiance of our fears, that the biggest strides in development are made — think astronauts exploring outer-space or architects designing the world's tallest skyscrapers. In healthcare too, clinical innovations that are proven effective can be life-saving, but innovative treatments are often met with skepticism.
It can take up to 20 years for clinical innovations to be put into practice and over 50% of these never make it into general usage. An estimated 80% of bio-medical research investment fails to make a significant impact in public health partly because of non-adoption rates.
Patient emotions of fear, disgust, and unfamiliarity are some of the many complex reasons for the low uptake of evidence-based clinical innovations. Other reasons include lack of knowledge transfer from clinical trials to practice, the power of status quo, and existing brand name recognition.
Vaccine hesitancy and fear of needles

When inoculation (the first form of vaccination) was discovered in 1722 to combat a smallpox outbreak in Boston, many doctors believed it went against “divine law,” to inoculate a deadly disease into an otherwise healthy person. Opposition was vehemently sustained until it became evident that the “unholy” process of inoculation could save lives (a 98% survival rate with vaccinations versus an 85% survival rate without it).
Vaccination is now the most effective form of preventative treatment for infectious diseases. It's administration, from birth to adulthood, is a standard healthcare process in most developed countries.
Yet fear and misinformation lingers still. An estimated 16% of the US population skips vaccination. With 25% of the population suffering from trypanophobia, a fear of needles is likely a contributing factor to non-vaccination. Yet vaccination risk is low, whereas the chance of getting the flu is 40–60% higher without the vaccine.
Causes of trypanophobia can vary, from a genetic influence to low pain tolerance, but one thing is certain: misinformation plays a significant role in legitimizing this fear, often leading people to refuse vaccination altogether. Educating patients on the benefits of vaccination from a medical point of view can reduce misguided fear and increase vaccination uptake.
Using empathy
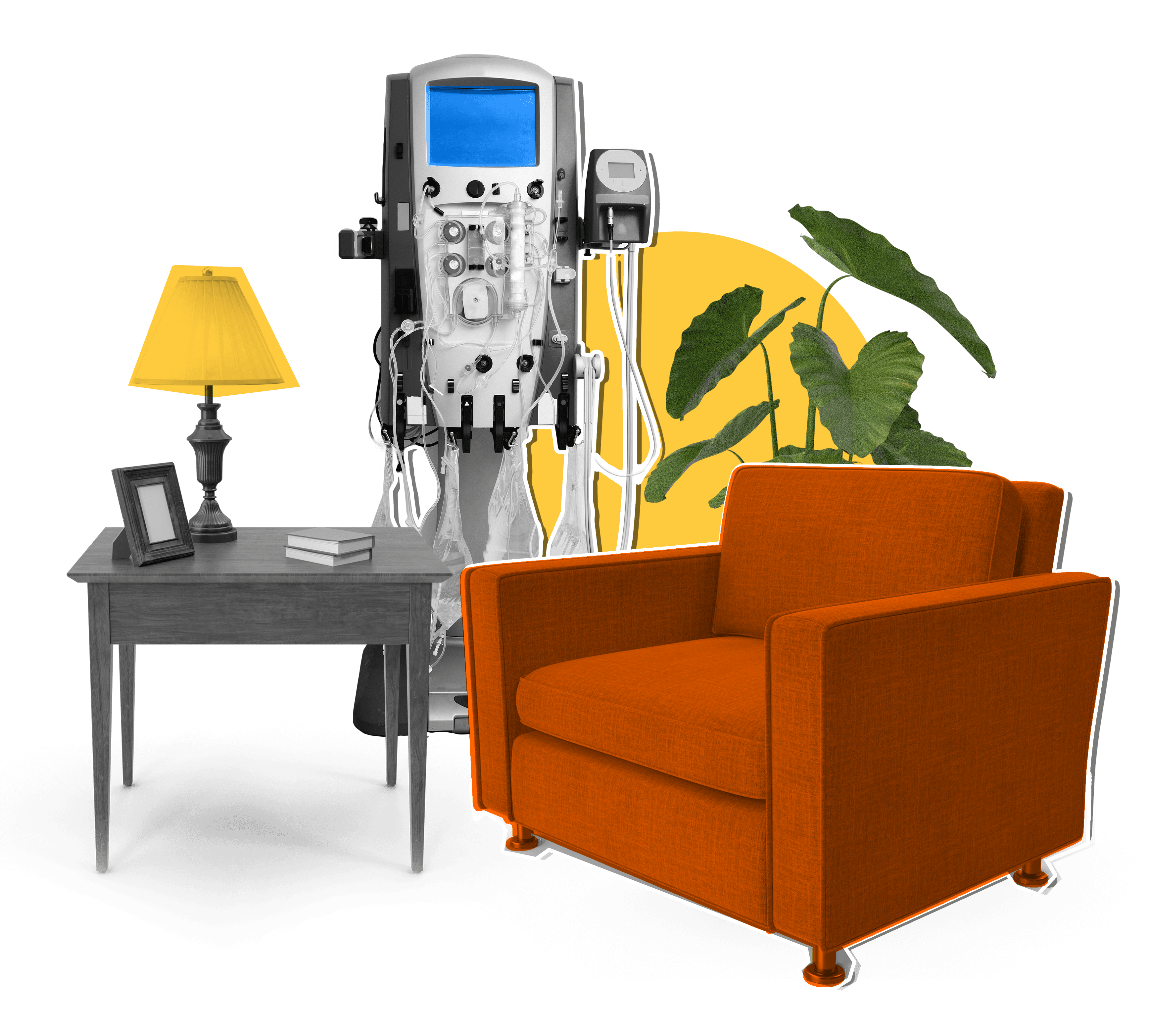
Healthcare providers can use empathy as an emotional pathway to treatment adoption and adherence. At-home dialysis, a treatment for chronic kidney disease (CKD), increases life-quality, likelihood of transplant, and prevents hospitalizations compared to in-clinic dialysis which requires a 4-hour-long tri-weekly procedure. In the US, hemodialysis is also insured by Medicare.
Despite these benefits, only 50% of patients choose at-home dialysis over in-clinic. “Fear that something could go wrong,” was cited as the #1 reason patients opted against at-home dialysis, according to a BEworks study. Deeper research found that misinformation about the complexity of the at-home procedure was a leading reason for patient fear.
Better informing patients about the set-up and benefits of the treatment itself can help dissuade patient fears. A supportive clinical environment where nurses can have one-on-one conversations with patients using an empathetic approach allows more informed decision-making on health and may increase at-home dialysis treatment uptake.
Shifting the “gross” scale
Disgust, a close relative of fear, can also hinder the uptake of new medications. When Canadian cough medicine brand Buckley’s rolled out their award-winning marketing campaign: “It tastes awful. And it works,” it was the perfect behavioral nudge.
Buckley’s used the pain vs. reward scale to convice their audience that symptom alleviation was well worth the medicine’s bad taste. Highlighting the pain versus reward trade-off in healthcare communications can offset the predisposed “Yuck!” response that makes patients hesitant to try or adhere to effective new treatments.
BEworks advisor Erick Roat weighs in on this, “in some ways, these emotions [fear and/or disgust] are a payment for the benefit. It’s about changing the ratio: shrinking the fear and growing the benefit.”
Motivating acceptance of the unfamiliar
 People are notoriously good at sticking to what is familiar to them. Routines are comforting because we know what to expect and they can guard us from potential losses, but also from its potential benefits.
People are notoriously good at sticking to what is familiar to them. Routines are comforting because we know what to expect and they can guard us from potential losses, but also from its potential benefits.
Two years after Benadryl was no longer recommended as the first line treatment for allergies, people still continued to reach for it over lesser known brands with fewer side effects like Claritin. People preferred to purchase a brand they were already familiar with, a process known as brand-name recognition.
Motivate instead of discourage health patients and they may be more willing to try new, evidence-based treatments, says Dan Ariely, Duke University professor and BEworks co-founder, when asked about treatment adherence and solutions.
Health and emotion: A symbiotic relationship

Medical treatments can dramatically improve the life quality of patients, but patient emotions of fear, disgust, and unfamiliarity can hinder their compliance with them. Acknowledging patient fears with empathy, leveraging the pain versus reward trade-off, and dispelling treatment misinformation can bring clinical innovation to routine usage faster and help patients lead longer, healthier lives.
At BEworks, we can help providers and policymakers better understand the psychological factors in healthcare adoption barriers and build behavioral strategies to increase the uptake of effective treatments.