

In many cases, involving more stakeholders in a medical decision carries a range of benefits: the physician may get better insight into their patient’s difficulties, capacities or resources, pitfalls can be avoided, tools can be discovered, and overall, a stronger plan can be crafted. So why wouldn’t this happen, to the fullest extent, every time?
We often get questions that are variations of something like: “Behavior X is better for everyone but doesn’t happen as often as it should. How can we change this?” The answer is usually heavily nuanced but can be boiled down to a few “usual suspects” that are blocking or creating “drag” on the behavior. Some common ones include:
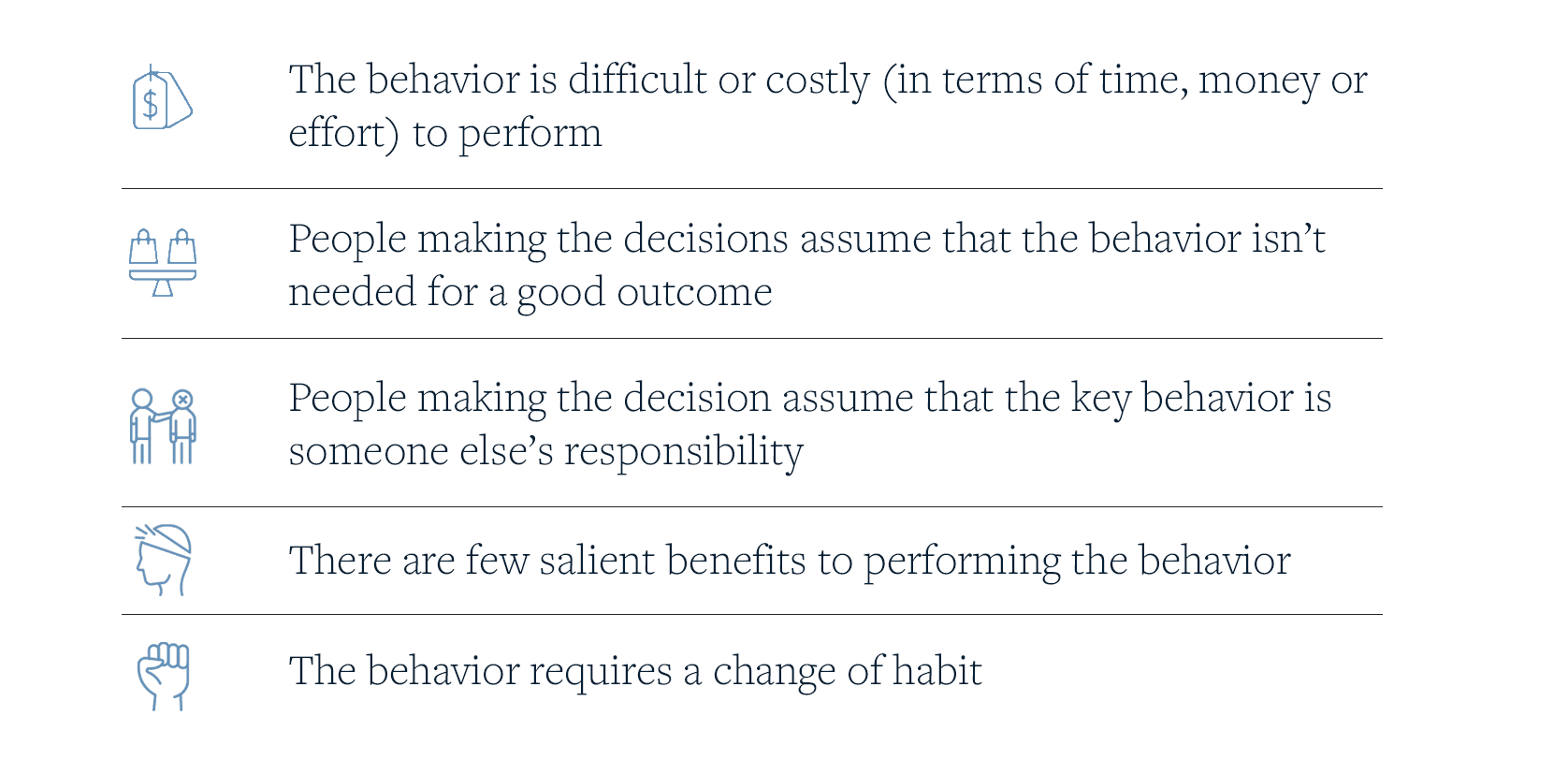
Looking at it from that perspective, we are often faced with the tall order of trying to encourage more people to perform a novel behavior, that is seen as costly or difficult and often perceived as an additional responsibility, without a strong sense of benefits in performing it. Awareness and education campaigns can help make people aware that a given behavior exists and can inform about benefits, but these steps are relatively weak in changing ingrained behaviors. We often need a set of interventions that help to reduce the “cost” and effort of using the behavior, reveal the benefits in personally salient ways, and to make it harder to sidestep the behavior. One powerful concept that opens the door to this kind of approach is the idea of altering the Choice Architecture involved in a given behavior. Choice Architecture is defined as “the physical and symbolic environment that faces decision-makers at the point where they make a decision”
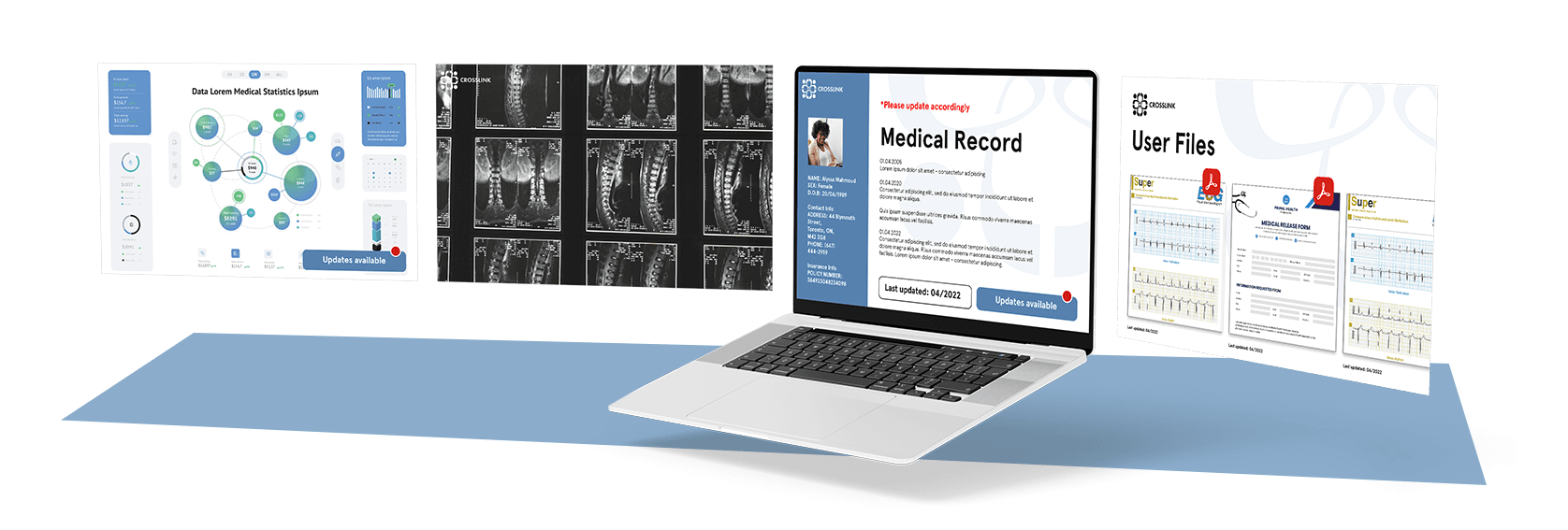
For example, over the past 20 years in the healthcare ecosystem, we’ve already witnessed the amazing benefits to medical care that have accrued from the Choice Architecture change represented by the electronic medical record. The EMR allows professionals and specialists, and sometimes family members or the patient themselves, to share information and collaborate in a patient’s care. The way the EMR is structured steers people’s behavior to add to and to use the record in a natural way: they review other professionals’ notes, engage in consultation, share results and post their findings to the record. As a thought experiment, imagine trying to achieve the same benefits to collaboration and information sharing using 1950’s-style technology and the different Choice Architecture that system represented. Without the Choice Architecture, represented by an EMR that creates a pathway for the desired behavior, we’d be relying on information, education, rewards and sanctions to try to get medical professionals to engage in the same collaborative behaviors that come naturally with the EMRs.
When considering ways to encourage patients to draw from the larger health ecosystem and their social networks in making their choices, it would be wise not to ignore opportunities to consider how Choice Architecture could be used to nudge desirable behaviors. We might imagine that the current Choice Architecture looks something like this: after several consults, a suggested treatment approach is presented by the physician, for the patient to approve. Let’s call this Choice Architecture “A”. Changes to Choice Architecture A that would encourage patients and physicians to consider other influences (we’ll call it Choice Architecture “B” ) might involve providing the patient with a guide or a personal health webpage that has spaces prompting them to consider input from relevant stakeholder groups and family members, with art and design to create the impression that a decision isn’t “complete” until several of these avenues have been explored. Depending on the resources available, communication with or information from these stakeholders could be set up as a default option that happens without (or with minimal) patient effort. We could even imagine a feature, in an online tool, where family members or doctors could post articles or comments relevant to the person’s medical journey.
There is a lot more to imagine about how Choice Architecture could be used to approach this problem; while we chose to use technology-driven alterations in imagining changes in the Choice Architecture, similar positive changes could be made focused on signage, the physical environment where decisions are talked about (and who is invited), the time-line of decision making, or even what the physician or others say to the patient about the decision-making process. As a start, comparing the two imaginary Choice Architectures we’ve created (A and B) is intended just to illustrate the potentially strong role of Choice Architecture to encourage a patient to consult additional stakeholder. Literally infinite types of changes to a given Choice Architecture are possible, with many possible ways to target the barriers to action so often encountered in this kind of situation.
References:
Hart, J., Yadav, K., Szymanski, S., Summer, A., Tannenbaum, A., Zlatev, J., Daniels, D., & Halpern, S. D. (2021). Choice architecture in physician-patient communication: a mixed-methods assessments of physicians' competency. BMJ quality & safety, 30(5), 362–371. Advance online publication. https://doi.org/10.1136/bmjqs-2020-011801
Mertens, S., Herberz, M., Hahnel, U. Brosch, T. (2022). The effectiveness of nudging: A meta-analysis of choice architecture interventions across behavioral domains. PNAS: Psychological and Cognitive Science, 119, https://doi.org/10.1073/pnas.2107346118
Acknowledgements:
We’d like to thank Jeff Fayer (ELIQUIS Consumer Director, Pfizer) and Karen Diaz (Senior Director of Innovation, Regeneron) for the early conversations and questions they posed that prompted the creation of this piece.